Hi All,
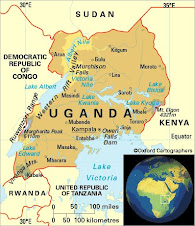
So this is my 4th week in Uganda and my 2nd week in Tororo. We started off the week on Monday in the women’s ward doing rounds. The first patient we saw was a 60 yo women with type 2 diabetes that was initially placed on insulin but had run out and came in with excessive thirst, urination, and neuropathy. It was interesting, because the wards are basically run by clinical officers (like a PA or NP) but there is supposed to be a doctor responsible for that ward and rounding on those patients. At Mulago, we saw the attending physicians coming 2-3 times a week….in Tororo we saw them come barely once a week, and the clinical officer basically does all the work. So, Dr. Welishe was brought to this patient in specific cause it was Diabetes, something the clinical officer was not as comfortable managing. You give the C.O. HIV, malaria, Tb, multiple other infectious diseases, they would have no problems. It is just interesting to see the differences in causes of morbidity and mortality! So Lisa and I had a lot to contribute with the Diabetes patient (ACE-I’s, education on foot care, urine proteins, ect) and we ended up changing her from insulin to metformin (her pancreas can still produce some insulin)
One of the more interesting patients of the day was a young girl, age 8, with anasarca (generalized edema and swelling all over the body). We questioned why this 8 yo was on the adult ward and realized that the pediatric ward was all children under 5 and everyone else goes to the adult wards. Dr. Welishe said that with the huge amount of disease affecting children under 5 and the high mortality rate for <5yo the peds wards are to swamped to take older kids. They don’t even have beds on the peds wards to fit kids bigger than 3 ft So this poor little girl probably had nephritic syndrome (where your kidney’s can no longer keep protein from draining out of your body in the urine). This rotation has been great, because even the #1 cause of nephritic syndrome in children is different her because of the frequency of infectious diseases. At the same time, she had a huge palpable spleen and renal mass. We aren’t sure yet what the renal mass is, but immediately I thought of a Wilm’s tumor, but Dr. Welishe mentioned that here they also have to think more about Burkitt’s lymphoma.
Another interesting patient was a young girl, 8 yo also, who had “fits” epilepsy and was brought in with an absolutely awful desquamating rash, with open ulcerations all over her body. As we were seeing the patient next door, see was cuddled up in a ball so small, I first questioned if she was missing the lower half of her body. She shamefully covered her self with her single sheet on the bed, with just a few inches of open ulcerated skin showing. When we finally saw her, you could see that the skin eruption involved her whole body including her eye lids that had sealed her eyes shut and her mouth to the point where she could not swallow and saliva was slipping down the outside of her mouth. The “sisters” nurses informed us that she had improved since yesterday. When questioning the family, we got an unclear history of whether she was treated with anti-malarials or anti-epileptic medications. This was Steven-Johnson syndrome, something I have seen 2 other times here in Uganda, but not nearly this severe. The rash is most likely from an anti-epileptic medication she received.
Some other interesting patients we saw included a epileptic women with 3rd degree burns on her breasts from falling into a cooking fire during a “fit”, a women with HIV wasting syndrome and severe obstructive jaundice and hepatomegaly which we placed on palliative care, a patient with probably typhoid fever, a women with a patellar tendon rupture for the past 3 mos! Interesting physical exam finding for the day was a seropositive women (HIV) with nodular hepatomegally. You could see the edge of her liver and the nodules with every breath and they became even more apparent on palpation.
We also recently saw a patient with herpes zoster (shingles). Immediately when he got shingles they gave him an HIV test, and the man was incredibly distraught cause he had shingles so he assumed he had HIV. When his test came back seronegative, he didn’t believe it. In Uganda, a patient with zoster, has HIV until proven otherwise. We had to convince he that he didn’t have to have HIV just because he had shingles. In the states we usually don’t think twice about shingles, unless there is something else to make us suspicious of HIV.
Some other notes about things I have learned. The hospitals often run out of many of the medications. This includes Tb drugs. Uganda has had no Tb medications since January (I may have mentioned this already) and I think is in the process of getting some more We talked to one doctor who when he has 3 patients who need Tb treatment, he fudges the numbers and says he has 6….the patients of this doctor have had there medications this whole time. Is this ethical? He is reducing the amount of resistant Tb by providing continuous treatment for his patients, on the other hand he is forging the numbers to get these medications, and this may causes a shortage somewhere else. Interesting ethical dilemma I think! Something else I learned is that when hospitals are out of amoxicillin, it costs 1,500 schillings from the pharmacies in town. This is the equivalent of 75 cents, yet, when the hospital runs-out a good majority of the patients can not afford it. This experience has really taught me the importance of taking to patients about their resources and what they can afford before prescribing medications or recommending certain studies. If you prescribe a medication, but it is to expensive so they never get it, you are really not helping them at all. I have also been noticing the shy nature of the women I have seen on the wards and in the clinic. Women rarely look any of the health care workers in the eye, are very quite, and only speak when spoken too. It is much more of a paternalistic, doctor knows best mentality, than what I am used to in the states. Just an observation.
Yesterday, we spent the day in the antenatal ward, labor and delivery. When we arrived with Dr. Welishe, we were greeted by the many midwifes. We soon learned that the last time the doctor responsible for the ward had rounded with the midwifes was March 18th, yes that’s right, over 1 month ago. Luckily, the midwifes know there stuff, but you could tell they appreciated the rounds with Dr. Welishe to learn more and think outside the box. I won’t talk about this too much, it was a lot of the same things you would see on a maternity ward in the US. It was interesting however to see how they combat HIV transmission from seropositive mothers to the newborns. During the mothers antenatal visits, the are given an antiretroviral for labor (if they are not already on) and an antiretroviral syrup for their newborn to take home with them. 85% of women in Uganda attend an antenatal clinic, however only 30% deliver by skilled mid-wives or doctors. By giving them the medications ahead of time, if they do deliver in the village, they can still do there best to prevent transmission of HIV to their newborn. The other big highlight was seeing a mother who was G13P12, great-grand-multiparous, that means it is her 13th pregnancy. I know that used to not be a big deal, but that was the highest I have seen. Listening and trying to count out the fetal heart tones with the fetoscope, 5 inch long “acoustic device” caused some challenges in comparison to the fancy Doppler heart tones we are used to hearing!
Today was Operating Theatre (OR), Lisa has been looking forward to this ;) When arriving to the door of the theatre, you immediately have to take off your shoes. Luckily I was informed of this and had my handy dandy socks with me. From there we were able to change into our scrubs and put on the huge white rain boots that we are allowed to wear in the OR, along with the cloth hats to cover our hair and the cloth masks for our face. The OR has one set of instruments that they have to sterilize between cases, so by the second case, the metal instruments were scalding hot from just being cleaned. Today there was a appendectomy, a hernia repair and a lipoma removal. Lisa, future surgeon, did the lipoma removal with some assistance from Dr. Welishe. I on the other hand, was much more interested in the anesthesia. The available medications included thiopental, succinylcholine, ketamine, diazepam, atropine, and ether as the inhalation anesthetic. I have never seen ether used, so I was eager to learn about it. On the second case I was able to do the intubation, and run the anesthesia. This consisted of hand ventilating through the case since there is not a ventilator Oh and also adjust the ether…it gave me something to do! By the last case, they had run out of sterile gowns, gauze, drapes, so from there, all other elective cases were put on hold until they could be replaced. It was a good day in the OR.
Well I will try to wrap things up, but I want to leave you with one story. A few months ago, Dr. Welishe was at the hospital when he received a phone call from one of his fellow doctors at the hospital who is responsible for the labor and delivery. This doctor said he was in the labor and deliver ward, and he had a patient with obstructive labor that needed to go to the OR for a c-section. The doctor mentioned that he was not feeling well and that he would appreciate if Dr. Welishe would do the case so he could go home and rest. Being the nice man he is, Dr. Welishe agreed. Immediately after the case, Dr. Welishe traveled to Mbale, 40 km away to pick something up. On the side of the road he saw this doctor waiting for a taxi to take him back to Tororo. Turns out, the doctor was never at the hospital, he had been at a private clinic 45 minutes away all day, to earn extra money and do tubal ligations. When a urgent case came in and he was not there…he called Dr. Welishe and said he was sick. After all this Dr. Welishe picked him up and gave him a ride back to Tororo with out a word.
So I leave you with that. With all the Swine flu, Lisa and I are anticipating an interesting return to the states since we are coming from London, so we will have to follow it closely.
Miss you all,
Crystal
Wednesday, April 29, 2009
Subscribe to:
Post Comments (Atom)
No comments:
Post a Comment